
This information is to help readers understand Pediatric Pancreatitis and the effects on children. Pancreatitis is an inflammatory condition of the pancreas (the long gland behind the stomach in the upper area of the abdomen). Pancreatitis is commonly misdiagnosed and it is important to be aware of symptoms, causes and major types. This condition is treatable with most conditions being a reversible process if treated early. For more information please review the Pediatric Pancreatitis research below.
Summary:
Research on the exocrine pancreas has traditionally been slow in making progress towards understanding and treating diseases, due in part to a lack of awareness about the disease as compared to other diseases with similar outcome statistics. As a result, research funding for exocrine pancreatic diseases has been low compared to other diseases (including endocrine pancreas diseases). Thankfully, recent advocacy efforts by organizations supporting cures for these diseases have been very successful at capturing the attention of the public and the government. These efforts, coupled with publicity surrounding the passing of well-known sufferers Steve Jobs and Patrick Swayze, have led to an increase in federal funding for pancreatic cancer and a resurgence in interest about other diseases of the exocrine pancreas. Though we still have a long road ahead and some catching up to do, hope is definitely on the horizon for those who suffer from these diseases.
Exocrine pancreas research can be broken up into two areas: laboratory based research and clinical research. Laboratory research typically consists of microscopic or genetic studies on cell growth, disease process, and cell death, while clinical studies are currently focused on improving therapies and diagnostic tools for healthcare professionals and measuring the effectiveness of existing therapies across the globe.
The primary goals of current research are:
- Unlock the mysteries of the genetic and biochemical components of exocrine pancreas physiology
- Discover new biomarkers that are more indicative of normal and abnormal pancreatic function
- Improve survival rates of certain diseases by improving diagnostic methods and technologies
- Improve treatment of pancreatic diseases by improving therapeutic technology
Please click on the links below to learn more about research:
Some Organizations and Journals Supporting Pancreas Research
American Pancreatic Association: Founded in the late 1960’s in an effort to promote communication and collaboration amongst clinical and basic research, the APA exists today as a professional society dedicated to advancing research towards a cure for pancreatic diseases. The APA also oversees the professional journal “Pancreas”.
National Pancreas Foundation: The NPF provides research grants and supports education for all those involved in the fight against pancreatic diseases. Though they have only existed for 13 years, some of their funding has helped researchers make significant progress in understanding the genetics behind the exocrine pancreas.
Pancreas Cancer Action Network: As a result of their own personal experiences with Pancreatic Cancer, PanCan’s founders were highly motivated to advance research and promote awareness of the disease and have been very successful in their short 13 years of existence. They award millions in research dollars per year, provide a network for patients and families suffering from the disease, and have been a champion of advocacy in Washington D.C.
Lustgarten Foundation: The Lustgarten Foundation is the largest private foundation dedicated to Pancreatic Cancer research. It was established in 1999 after the death of a Cablevision executive Marc Lustgarten and has been underwritten by Cablevision, allowing 100% of donations to fund research. Lustgarten also helped establish the Pancreatic Cancer Research Consortium, a collaborative consisting of some of the country’s top cancer centers and universities
Pancreas Specific Journals:
Pancreas: The official journal of the American Pancreatic Association, Pancreas was first printed in 1986 and is currently published by Lippincott, Williams, and Wilkins. Pancreas publishes both basic and clinical research, as well as surveys and state-of-the-industry information.
Pancreatology: Pancreatology is the Journal of the International Association of Pancreatology and has been in print since 2001. This journal publishes research, case studies, and reviews of current progress in the fight against pancreatic diseases.
Causes of Exocrine Pancreas Diseases
“It is common error to infer that things which are consecutive in order of time have necessarily the relation of cause and effect.”
Jacob Bigelow, M.D.
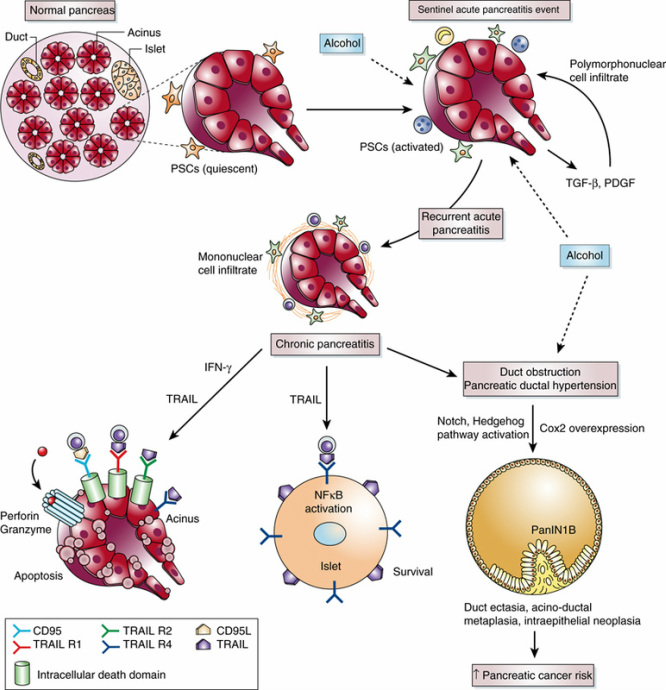
Illustration of the hypothesized causes and progression of various pancreatic diseases. Can we definitively say what is cause and what is effect (36)?
There are numerous causes of diseases in the exocrine pancreas, and one described disease can have a very different source from another.
Pancreatitis, for example, is a general inflammation of the pancreas whose source could be bacterial, cancerous, or mechanical, and even self inflicted by alcohol abuse or overeating. On the other hand, Cystic Fibrosis is a genetic disorder (covered in some detail on the mathematics page) that can lead to pancreatitis but is definitely not the result of some external source. This makes diagnosis all the more challenging and much improvement is needed in our current testing capabilities to more definitively determine early stage sources of diseases before they progress too far.
Pancreatitis: By far the most common disease of the pancreas, this very broad term can be used to describe a wide range of conditions whose causes may or may not be known. We currently classify pancreatitis as either acute or chronic, and sometimes hereditary. Our discussion here will cover acute and chronic pancreatitis. However, it is notable that we use such a general term as one of the primary medical classifications of pancreatic disease; perhaps even an indicator of how little we really know about the mysteries underlying the pancreas.
Acute Pancreatitis: The primary causes of acute pancreatitis are alcohol abuse and stones in the outflow path. Alcohol has a number of inflammatory effects within the pancreas. One theory is that heightened levels in the digestive tract cause the pancreas to work harder than normal, and since the pancreas directly metabolizes alcohol, the oxidative stresses from hyperactivity may cause cell membranes to weaken. Eventually this could cause secretion of pancreatic juices intracellularly, with the pancreas effectively eating itself.
Gallstones can also cause a fluid “backup” in the pancreas by obstructing ducts downstream of the outflow, and the digestive enzymes build up and put pressure on the cell walls within the pancreatic duct and acini (covered in detail in the Mathematics section). This too can cause leakage of the digestive enzymes into the intercellular space, but it can also put stress on the walls of the duct and potentially form a cyst if distention creates a weak point.
That’s really going straight to your Pancreas (37).
Chronic Pancreatitis: The causes of chronic pancreatitis can be the same as the causes of acute pancreatitis, but chronic pancreatitis is defined as a recurring condition that damages the pancreas in a more permanent way. In fact, repeated bouts of acute pancreatitis can lead to chronic pancreatitis. Chronic pancreatitis also typically has a longer duration than acute pancreatitis, is typically associated with genetic or long term disease conditions like Cystic Fibrosis and Pancreatic Cancer. High levels of calcium or lipids and hyperparathyroidism have also been associated with chronic pancreatitis (38).
Pancreatic Cancer: The causes of this deadly disease are still very much under investigation, but recent attention surrounding it has given birth to a number of fantastic research initiatives that aim to uncover the genetic and biochemical basis for its beginnings. What we know for certain is that it follows a similar pattern to other cancers with respect to DNA mutation and uncontrolled growth, so most patients are advised to eliminate known carcinogens from their lives (i.e. cigarettes and overconsumption of unhealthy foods). Cancer research in other areas is aiding the fight against pancreatic cancer by way of translational concepts.
Diagnosis of Exocrine Pancreas Diseases
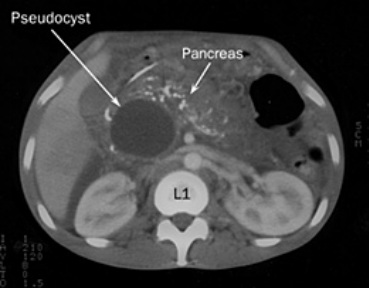
CT (Computed Tomography) scan showing a transverse
“slice” of the abdomen containing a pancreatic pseudocyst,
viewing from the feet (7).
http://www.youtube.com/watch?v=OS5lMaK8jFE&feature=player_embedded
An overview of the EUS (Endoscopic Ultrasound) procedure used for diagnosis of many pancreatic diseases, from Johns Hopkins (6).
Diagnosis of exocrine pancreatic diseases typically involves a variety of imaging and endoscopy equipment due to the depth of the pancreas within the body. While acute problems typically present with pain, the disease process can be slow and early symptoms of disease may be difficult to definitively associate with the pancreas. Researchers are currently working to give us tools to better diagnose these diseases sooner, but one of the biggest challenges in dealing with them is that we don’t typically find them until late in their developement. Thankfully, the technology we currently have does a fairly accurate job of locating pancreatic diseases at this stage. The process of diagnosis includes:
- Physical examination
- Blood tests (though these may not necessarily provide definitive results)
- Imaging Tests, such as X-Ray, Magnetic Resonance Imaging(MRI), or Computed Tomography (CT)
- Biopsy to determine tissue contents (typically for ruling out infection or cancer)
- Other tests such as fecal chemistry, pancreatic stimulus response tests (secretin), and sphincter manometry
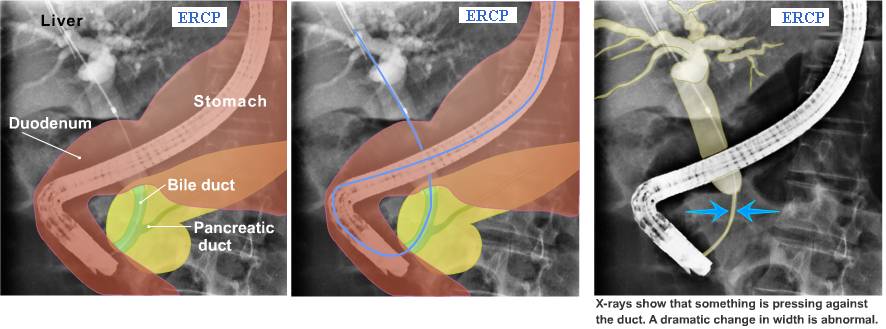
Physicians will check for anatomical abnormalities using imaging equipment, and look for hallmarks of infection and other diseases in blood tests. Biopsies are done under guidance of imaging equipment, and can be performed percutaneously. However, the easiest access for taking tissue samples is via natural orifice approaches such as Endoscopic Retrograde Cholangiopancreatography and Endoscopic Ultrasound. Both of these procedures utilize a device called an endoscope, which is inserted in the patient’s mouth and advanced to the duodenum where the pancreatic and/or common bile ducts are accessible via catheters and instrumentation (similar in technical detail to cardiac angiography).Bile duct obstruction at the pancreas (39)
ERCP and EUS are becoming more common as diagnostic tools due to their high degree of specificity and relative safety compared to percutaneous methods. These procedures can be highly technical and equipment is costly, so they are currently performed in an academic or pancreas and biliary specialty center where a greater number of experienced specialists are available. One of the benefits of this technology is that treatments for certain conditions such as blockages or strictures can be performed immediately following diagnosis, which reduces repeat visits and can save a trip to the operating room.
Effects of Exocrine Pancreatic Diseases
The effects of exocrine pancreatic disease are typically the development of more advanced pancreatic diseases, and though the cause-effect relationship is not linear it is linked. Pancreatitis can lead to the development of pancreatic pseudocysts, fluid outcroppings within the pancreas as a result of narrowing or blockage of the outflow of pancreatic secretions. All pancreatic diseases have been linked to an increase in the risk for pancreatic cancer, and acute pancreatitis has been linked to chronic pancreatitis.
On a more widespread scale, malfunctions of the pancreas cause pancreatic insufficiency, which results in challenges with digestion of food. This can lead to malnutrition and problems in the intestines caused by passage of improperly digested food. Pancreatitis can also cause diabetes (due to Islet cell damage), kidney damage, and problems with other organs in the circulation if acinar cells are damaged and their contents find their way into the circulation.
In some cases, exocrine pancreatic diseases can lead to death if treated too late in their progression. Pancreatic pseudocyst rupture or pancreas rupture are serious conditions requiring emergency medical care, and pancreatic cancer currently has a relatively low survival rate due to its rapid spread and late detection within the body. However, new research is changing the playing field and reducing the severity of these effects.
An extreme case of abdominal diseases involving the pancreas.
Drug-Based Treatment of Exocrine Pancreatic Diseases
Drug-Based treatment of pancreatic diseases is usually targeted at supplementing the malfunctions of the pancreas and controlling the pain associated with pancreatitis. In cases involving infection, antibiotics may be prescribed. Pancreatic cancer may be treated with chemotherapy drugs or drugs targeted at stopping or slowing cell division.
Supplemental Enzymes: These drugs typically consist of supplemental lipase, amalyaze, and protease prescribed in quantities that will help make up the difference in the insufficiency as diagnosed (usually based on weight loss and the consistency, regularity, and contents of the fecal matter). Supplements are usually well tolerated with relatively low incidence of side effects, the there are still some questions as to the efficacy of certain coatings and mechanisms of action, causing the FDA to release standardization requirements for trials (40). Some examples of brand name drugs are Creon, Ultrase, Zenpep, Zymase.
Pain Medications: Depending on the severity and duration of pain, drugs can range from typical over the counter types of acetamenophin or ibuprofen to heavy-duty prescriptions such as hydrocodone or even morphine. Some brand names are Motrin, Vicadin, and Demerol. Side effects are wide ranging and overdosing can lead to problems with other endocrine functions and even death. A physician’s orders should be strictly followed when using any medications, and most of these should not be taken with alcohol (though pancreas patients should already be eliminating alcohol consumption).
Pancreatic Cancer Drugs: Drugs used to treat pancreatic cancer typically belong to the general family of cancer treating and/or chemotherapy drugs. Some specific names include Fluorouracil, Mitomycin C, Erlotinib Hydrochloride, and Gemcitabine. Most work by acting on DNA and attempting to prevent specific cell replication, but typically have a system-wide effect. Others may act on blood vessel growth hormones (trying to starve the tumor by preventing its blood supply) These drugs have similar side effects to other cancer drugs, which includes bone marrow suppression/toxicity, immune system issues, kidney issues, lethargy, diarrhea, and higher risk of illness or infection. Newer drugs that target cancer cells more specifically such as Erlotinib have been developed as a result of genetic research and may have less side effects than traditional chemotherapy (42).
Medical Device Based Treatment of Exocrine Pancreas Diseases
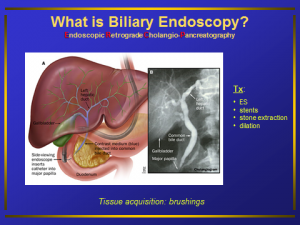
ERCP, a device based treatment (23)

Radiation therapy for cancer treatment (45)
Medical device based treatment of exocrine pancreatic diseases falls into 2 main categories:
Radiation Therapy (using ionizing imaging equipment)
Endoscopic Therapy (using endoscopes and catheters)
For many years, Physicians seeking a medical device-based solution for exocrine pancreatic diseases have had to adapt technologies from other disciplines such as urology and pulmonary medicine to allow them to access and , Medical device based treatments for exocrine pancreas diseases are numerous.
Surgical Treatment of Exocrine Pancreatic Diseases
Surgical treatment of these diseases has been the traditional standard when cases reach their critical stage, but in recent years it has been positively supplemented by natural orifice procedures such as ERCP and EUS. However, when removal of part or all of the organ is required, surgery is still the primary option for patients. Surgery for rupture of pancreatic tissues can be life-saving, and is currently still the only option for treatment. Surgery is broken into two categories: minimally invasive surgery (typically called laparoscopic) and open (or general) surgery.
http://www.youtube.com/watch?v=4Zxvm3MSb8k&feature=player_embedded
The Whipple, Courtesy Johns Hopkins (43).
General Surgery: General Pancreas surgery involves opening the abdomen via incision and dissecting tissue away to access the pancreas. Due to its location, many pancreas operations are challenging and time consuming for surgeons, and experience in pancreatic surgery is directly tied to patient outcomes.
Laparoscopic Surgery: Also known as minimally invasive surgery, laparoscopic procedures are performed using video imaging equipment including specialized cameras and optics called laparoscopes, as well as instruments and accessories designed to be inserted through a relatively small hole. Incisions are usually less than 1 inch, and recovery time for patients can be shorter. Pancreas resections, removal of pseudocysts, and stone removal can be performed laparoscopically, but due to challenges caused by the anatomical location of the pancreas, some surgeons may still perform these procedures open. With the widespread adoption of surgical robotics for laparoscopic procedures in general, there has been new interest in the application of this technology to pancreas surgery (44).
Pancreatoduodenectomy: The Whipple is an example of an open surgical procedure (though it can be performed laparoscopically). This procedure involves removing part of the head of the pancreas and is typically done to remove a pancreatic tumor and subsequently eliminate obstruction of the pancreatic outflow. Whipples take several hours and are considered high-risk operations because they involve removal of the duodenum/gallbladder, dissection near major blood vessels and removal of others, removal of part of the bile duct, and then reconnection of remaining bile duct and stomach to the jejunum. Patients undergoing this procedure typically are placed in the ICU, and hospitalization for around a week can be expected. Patients with pancreatic cancer that has spread to other areas are not considered candidates for this procedure.
Total Pancreatectomy and Pancreatic Transplant: These procedures involve removal of the entire pancreas, and are rare and typically performed at academic or large medical centers. Patients must be on a number of supplements and drugs to live without a pancreas, and these procedures may not be indicated for people with cancer.
http://www.youtube.com/watch?v=466HT8JuGtE&feature=player_embedded
Robotic Pancreas Operations: The Future for MIS(44)?
Partial Pancreatectomy and Cyst Removal: These procedures may be performed laparoscopically, and are typically done by surgeons experienced in this approach. Like the Whipple, they involve removal of part of the pancreas and major dissection but may not need to involve removal of the duodenum or other organs. This reduces risk for the procedure and also reduces patient recovery time.
Many surgical procedures have been proven to increase survival rates for patients with progressive disease, but as with any surgery there are risks that should be weighted with the help of expert physicians who specialize in pancreatic treatment to ensure the appropriate outcome for the patient.
Anatomy and Physiology of the Exocrine Pancreas
Video showing the basic anatomy and physiology of the exocrine pancreas, as well as some disease states (27).
Though the pancreas is primarily thought of as the insulin factory of the body, the bulk of its geometry is associated with its exocrine digestive features. Its functional unit is the Acinus, and it collectively secretes a variety of digestive enzymes that aid in the breakdown of proteins, lipids, carbohydrates, and other food components.
Gross Anatomy:
The pancreas is about 6 to 8 inches long and 1 to 2 inches wide, and lies in the abdomen just behind the stomach. It connects to the duodenum just below the stomach where its digestive “juices” are secreted. We break the pancreas up into 5 basic geometric regions as follows:
- Tail
- Body
- Neck
- Head
- Uncinate Process
The pancreas takes its blood from the pancreaticoduodenal arteries and the splenic artery, and returns it through the splenic and superior mesenteric veins.
Zooming Into Form and Function:
If we sliced a section out of the pancreas so we could see under the “hood” of the outer layers of tissue (below), we would find the main pancreatic duct and likely also find the common bile duct which joins the liver and gallbladder drainage to the pancreas. This is an obvious anatomical “choke point”, and its importance will be revealed in the disease process discussion. Under magnification, we would find the Acinar cells, which produce digestive enzymes that flow out of the main pancreatic duct and into the duodenum. The pancreatic duct is bounded by the duct cells, which secrete a bicarbonate solution to help neutralize the stomach acid on its way to the small intestine. The digestive enzymes secreted by the pancreas are not activated until they reach the small intestine.
A view inside the Exocrine Pancreas (25).
Micro-slice of an Acinar Cell showing some of its anatomy (26). The round nucleus is clearly visible in the middle of the cell, and it is surrounded by a host of organelles including a massive Endoplasmic Reticulum. The large form of Acinar ER fits the cell’s function as the greatest secretor of protein in the human body. The cell secretes these digestive enzymes via exocytosis of secretory vesicles (shown in black), and is activated by mechanisms that are not yet fully understood(24).
Tracing the Juice Flow:
The overall goal of the secretions is the breakdown of food, but the details of this process are a bit beyond the scope of this site. However, the Florida Institute for Human and Machine Cognition has done a nice job putting the basics together in a flow diagram. Read on if you dare!
Logical diagram of the functional result of Acinar cell secretions. (28)
Ironically (or perhaps appropriately), this drawing was made in the state known for its orange juice!
Control Systems of the Exocrine Pancreas
A diagram illustrating the afferent and efferent vagal pathways for pancreatic function. (24)
“The regulation of the secretory function of the pancreas by numerous hormones suggests that there are multiple and perhaps redundant signals governing the control of this important organ. Understanding these diverse pathways is essential to the treatment of pancreatitis, diabetes and obesity.” (29) – Dr’s Liddle and Chandra, Duke University Hospital, 2009
The control system for the exocrine pancreas consists of two primary mechanisms, Neural control and Endocrine control. Once thought to be somewhat separate in their actions on the system, new research is showing that as with many biological systems, there is a fair amount of interplay and the boundaries between regulatory actors may be much more blurry than originally postulated (29). Though the exact method of actions are still under investigation, we can currently make the following general observations:
- Cholecystokinin (CCK), secreted by the duodenum in response to food, appears to directly act on Acinar cells and promote secretion of
digestive enzymes by the exocrine pancreas - Secretin (the first named hormone in the body) from the small intestine stimulates the duct cells in the pancreas,
causing them to produce bicarbonate which helps neutralize stomach acid. - The sight, smell, and taste of food is the major external stimulus that begins the process of pancreatic secretion via
neuroendocrine pathways, and accounts for about 50% of the rate of secretion of exocrine pancreatic digestive enzymes (1).
We are hopeful that current ongoing research will further elucidate the control mechanisms for this system, which will allow us to better understand and treat their malfunctions.
Mathematics associated with physiology
“The utility of mathematics lies in its ability to represent and analyze seemingly chaotic raw data in a way which can yield academically or medically relevant information to the inquiring researcher or clinician.”
Andrew Shiels, Biomedical Engineering Researcher, University of Texas at San Antonio
The mathematics associated with exocrine pancreatic physiology can be complex, and it would take a volume of books to attempt to model every process taking place within this amazing organ. From a high-level viewpoint, we represent these processes with 2 main groups of equations as categorized by 2 basic physiologic functions of the pancreas, and take special cases to demonstrate application:
- Excrete Digestive Juices from the Cells: Cell membrane conductance and exchange equations
- Pass the Digestive Juices into the Duodenum: Flow and basic diffusion equations
Some of the material on this page make the assumption that the reader has a solid understanding of physiological equations, so we do not attempt to explain every variable presented here.
Note: we recognize neuroendocrine functions i.e. signaling diffusion and neurotransmitter flux and flow are important, but are not covered here for brevity.
Cell Membrane Exchange – Ductal Cells and the CFTR
Ion/Fluid Exchange in Duct Cells: Concentration of pancreatic juices is critical to the breakdown of food, and this concentration is dependent on a number of triggering mechanisms which are still being studied. However, we can make some assumptions about pancreatic cells based on the vast amounts of information obtained from basic cellular conductance experiments, so our membrane conductance equations and ion exchange equations definitely apply in this environment(1):
Diagram of ion exchange in a pancreatic ductal cell (24). Chlorine/Bicarb exchange is a known governer of flow rates of pancreatic juices in ductal cells (30). One contributor to issues with outflow is malfunctions or defects of the CFTR (Cystic Fibrosis Transmembrane Regulator). If duct secretions are limited by the action of this pump, the pancreatic juice becomes much thicker and denser, which challenges flow and solubility characteristics, potentially contributing to pancreatitis. Though known genetic mutations are a potential cause, recent studies are revealing previously undocumented genetic mutations which could be linked to this malfunction (31).
In 1999, Dawson et.al. took these equations and applied them to the the CFTR in general. Their work details the electrodiffusion of an anion channel as applied to chlorine conductance, which is particularly important in discussions about CFTR function and contribution to overall pancreatic fluid output. The discussion involves modeling the channel as a 2 Barrier 1 Binding Site passage, and begins by taking the simplest forms of Ohm’s law and doing a Feher-esque (1) derivation of predictive equations for passage of ions through the channel. Some of the highlights are taken directly from the article, and do a nice job of explaining how we can use mathematics to represent these concepts (32):
“If more than one permeant ion is present, E rev is the voltage at which the net current due to the algebraic summation of all permeant ion fluxes is zero.”
“In this condition, the channel is occupied virtually 100% of the time, and throughput is limited by the rate of exit of ions from a loaded channel.”
“The permeability of the N-P channel to an ion i is given by Equation 30 where A is the channel area, βi is the channel/bulk solution partition coefficient, D i is the intracellular diffusion coefficient, and Δx is the length of the channel.”
“Thus, for any permeability ratio, say Pj/Pi , we obtain the result that permeability ratios are not sensitive to ion binding.”
Bulk Pancreatic Fluid Flow – Gallstones and the Ampulla of Vater
The Pancreas produces approximately 1 to 2 liters of digestive enzymes per day on average, in a relatively non-linear fashion. In many pathophysiological conditions, problems with the flow of fluid are caused by blockages at the end of the duct. These blockages can build up over time, as in pancreatic cancer, or they can be nearly instantaneous as in the case of cholesterol deposits forming gallstones that pass down the bile duct and block the pancreatic outflow at the Ampulla of Vater. Below we undertake an original exploration of time-based effects of a gallstone causing complete blockage of pancreatic outflow.
The Duct as a Tube: Pancreatic outflow through the duct can be modeled using the principles of tubal fluid flow, which are governed by fluid flow and pressure laws (including Poiseuille’s and Laplace). The diameter of the pancreatic duct varies from head to tail(34), and the length of the duct is variable and dependent on the individual (36), but we take averages from study data to solve the equation for the time it would take to fill the pancreas given complete blockage of the duct:
Gallstone blockage at the Ampulla of Vater, at the end of the pancreatic duct (33).
4.5 minutes is an amazing result and helps explain why many cases of pancreatitis are acute. Pressure would begin to rise once the duct is full, and pain would result. Though we made a number of assumptions to get our answer, changing the numbers to maximum values and even allowing for some dilation of the duct (which happens to attenuate the pressure) would not change the time significantly. Since the values of flow are not linear but peak after eating, this helps explain why digestion can trigger acute “attacks”. Even if we doubled the volume of the duct (accounting for space in the branches) it would still only double the time.
References Cited
Giving credit where credit is due; this Resource Page would not have been possible without the following resources:
- Feher Quantitative Physiology
- Exocrine Pancreas book http://www.ncbi.nlm.nih.gov/books/NBK54128/
- USC Surgery info http://www.surgery.usc.edu/divisions/tumor/PancreasDiseases/web%20pages/PANCREATITIS/what%20is%20acute%20pancreatitis.html
- Math modeling of cell http://www.math.pitt.edu/~bard/pubs/pancreas.pdf
- NIH NIDDK http://www2.niddk.nih.gov/Research/ScientificAreas/Pancreas/
- Johns Hopkins EUS Video: http://pathology.jhu.edu/pc/cyst/video.php
- CT of pseudocyst: https://gi.jhsps.org/Upload/200802291655_2963_000.jpg
- NIH National Library of Medicine http://www.nlm.nih.gov/medlineplus/pancreaticdiseases.html
- UCSF Department of Transplant http://transplant.surgery.ucsf.edu/conditions–procedures/chronic-pancreatitis.aspx
- Mauna Kea/Cellvisio http://www.cellvizio.net/
- Cell Visio Research: Konda, V. J., Aslanian, H. R., Wallace, M. B., Siddiqui, U. D., Hart, J., & Waxman, I. (2011). First assessment of needle-based confocal laser endomicroscopy during EUS-FNA procedures of the pancreas. Gastrointest Endosc, 74(5), 992–1000.
- Herlev Hospital clinical trial of Cellvisio for examination of pancreatic masses http://clinicaltrials.gov/show/NCT01734967
- American Pancreatic Association http://american-pancreatic-association.org/
- National Pancreas Foundation http://pancreasfoundation.org/
- Pancreas Cancer Action Network http://pancan.org/
- Lustgarten Foundation http://www.lustgarten.org/
- Pancreas Journal http://journals.lww.com/pancreasjournal/pages/default.aspx
- Pancreas SEM Image: http://images.fineartamerica.com/images-medium-large/4-pancreas-tissue-sem-steve-gschmeissner.jpg
- Gastrointest Endosc. 2013 Nov 22. pii: S0016-5107(13)02222-0. doi: 10.1016/j.gie.2013.07.054. [Epub ahead of print]
Holmium-yttrium aluminum garnet laser lithotripsy in the treatment of biliary calculi using single-operator cholangioscopy: a multicenter
experience (with video). Patel SN, Rosenkranz L, Hooks B, Tarnasky PR, Raijman I, Fishman DS, Sauer BG, Kahaleh M. - Pancreas Gross Anatomy Image: http://health-7.com/imgs/20/8138.jpg
- Pancreatic Cancer Survival Stats (ACS) http://www.cancer.org/cancer/pancreaticcancer/detailedguide/pancreatic-cancer-survival-rates
- Spyglass Reuters Press Release http://www.reuters.com/article/2011/05/04/idUS257036+04-May-2011+PRN20110504
- “The Role of Endoscopy in Pancreatic Diseases”, UTHSCSA Grand Rounds 2010,, Patel, SN
- The Exocrine Pancreas. Pandol SJ. San Rafael (CA): Morgan & Claypool Life Sciences; 2010
- Pancreas Slice Image: http://o.quizlet.com/i/vfPKxCKhKlcYyzjZRVJ35A.jpg
- Pancreatic Acinar Cell http://www.diapedia.org/img_cache/markdown_lightbox_7ce6e2ec071d2e866658b430e28c00e796fe0f45-570a3.jpg
- Role and Anatomy of Pancreas video courtesy National Pancreas Foundation: http://pancreasfoundation.org/spa-en/#!/list/animation
- Diagram of Exocrine Pancreas Logical Physiology courtesy Florida Institute for Human Machine Cognition http://maaz.ihmc.us/rid=1203829070234_2017343929_31845/20.%20Exocrine%20Pancreas.cmap
- Chandra R, Liddle RA. Neural and hormonal regulation of pancreatic secretion. Curr Opin Gastroenterol. 2009;25:441–446.
- Regulation of CFTR chloride channel macroscopic conductance by extracellular bicarbonate
Man-Song Li, Ryan G. Holstead , Wuyang Wang, Paul Linsdell
American Journal of Physiology – Cell Physiology Published 1 January 2011 Vol. 300no. C65-C74DOI: 10.1152/ajpcell.00290.2010 - Minerva Pediatr. 2013 Dec;65(6):669-72. Brand new SPINK1 and CFTR mutations in a child with acute recurrent pancreatitis: a case
report. Terlizzi V, De Gregorio F, Sepe A, Amato N, Arduino C, Casale A, Majo F, Tomaiuolo R, Castaldo G, Raia V.
Source: Department of Pediatrics University of Naples Federico II, Naples, Italy – terlizzivito@libero.it. - Dawson, David C., Stephen S. Smith, and Monique K. Mansoura. CFTR: Mechanism of Anion Conduction. Physiol. Rev. 79, Suppl.:
S47–S75, 1999 - Gallstones in the Ampulla Pic: http://www.ddc.musc.edu/public/symptomsDiseases/diseases/pancreas/gallstones.cfm
- Measurement of Pancreatic Duct Diameters: J Clin Ultrasound. 1983 Jan;11(1):17-22. Pancreatic duct diameter: sonographic measurement in normal subjects. Hadidi A.
- Mymensingh Med J. 2011 Apr;20(2):298-302. The length of main pancreatic duct in Bangladeshi cadaver at different age
groups. Ara S, Shahriah S, Begum S. Source: Department of Anatomy, Dhaka Medical College, Dhaka, Bangladesh. - Pancreatic Disease Progression Image: http://www.nature.com/labinvest/journal/v89/n5/images/labinvest200919f1.jpg
- Drunk guy cartoon: http://uploads.neatorama.com/wp-content/twaggies/2012/05/Twag_0075.jpg
- ADAM Medical Encyclopedia, 2010 Chronic Pancreatitis http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001268/
- ERCP imaging of duct blockage http://www.aboutcancer.com/pancreas_ercp_jhu.jpg
- Clin Exp Gastroenterol. 2011; 4: 55–73. Published online 2011 May 4. doi: 10.2147/CEG.S17634 PMCID: PMC3132852
Enzyme replacement therapy for pancreatic insufficiency: present and future Aaron Fieker,1 Jessica Philpott,1 and Martine Armand2 - NCI list of Pancreatic cancer drugs: http://www.cancer.gov/cancertopics/druginfo/pancreaticcancer
- American Cancer Society http://www.cancer.org/cancer/pancreaticcancer/detailedguide/pancreatic-cancer-treating-chemotherapy
- Hopkins Whipple video: http://www.hopkinsmedicine.org/kimmel_cancer_center/centers/pancreatic_cancer/treatments/whipple_procedure.html
- Minerva Chir. 2011 Dec;66(6):603-14. Robotic pancreatic resection: how far can we go?
Buchs NC, Volonte F, Pugin F, Bucher P, Jung M, Morel P. Source Department of Surgery, University Hospital of Geneva, Geneva, Switzerland. nicolas.c.buchs@hcuge.ch - Rad therapy image: http://radiation-therapy-info.com/wp-content/uploads/2012/08/radiation-therapy.jpg
Disclaimer and notes: I have attempted to reserve all rights to property and content, legal and intellectual, and do not claim ownership of any works on this site other that my own words used in its making. I have no desire to make money from this site, and it was built voluntarily and without funding from any sources. My goal is to learn and raise awareness about diseases of the exocrine pancreas in hopes of improving the outlook for patients, having been inspired by many of them and motivated by the fantastic doctors who treat them. Please post any comments or concerns about the site on my blog page.
A very special thanks to Dr. Sandeep Patel and my wonderful wife for providing feedback and material, as well as coffee!




